In the spring of 2020, COVID-19 travel restrictions and quarantine requirements threatened to indefinitely suspend Dr Jose Estevez’s vision care service to a remote Australian community. He and his nurse practitioner partner selected QuickSee to develop a new practice to maintain the community’s access to vision care. “It was just what we needed for telehealth during the COVID peak,” said Dr Estevez.
Prior to the pandemic, Adelaide-based Dr Estevez visited the community, which is almost 900km (560 miles) from the nearest tertiary hospital, twice a year to see patients and make prescriptions for glasses. “My local partner had a lot of people who needed glasses, and there was nothing we could do. It could have been a year before I could go back, so we embarked on an intense search for a solution. I discovered QuickSee in a journal article and it showed good results.” Reading the literature on QuickSee, he found the results “strong and convincing.”
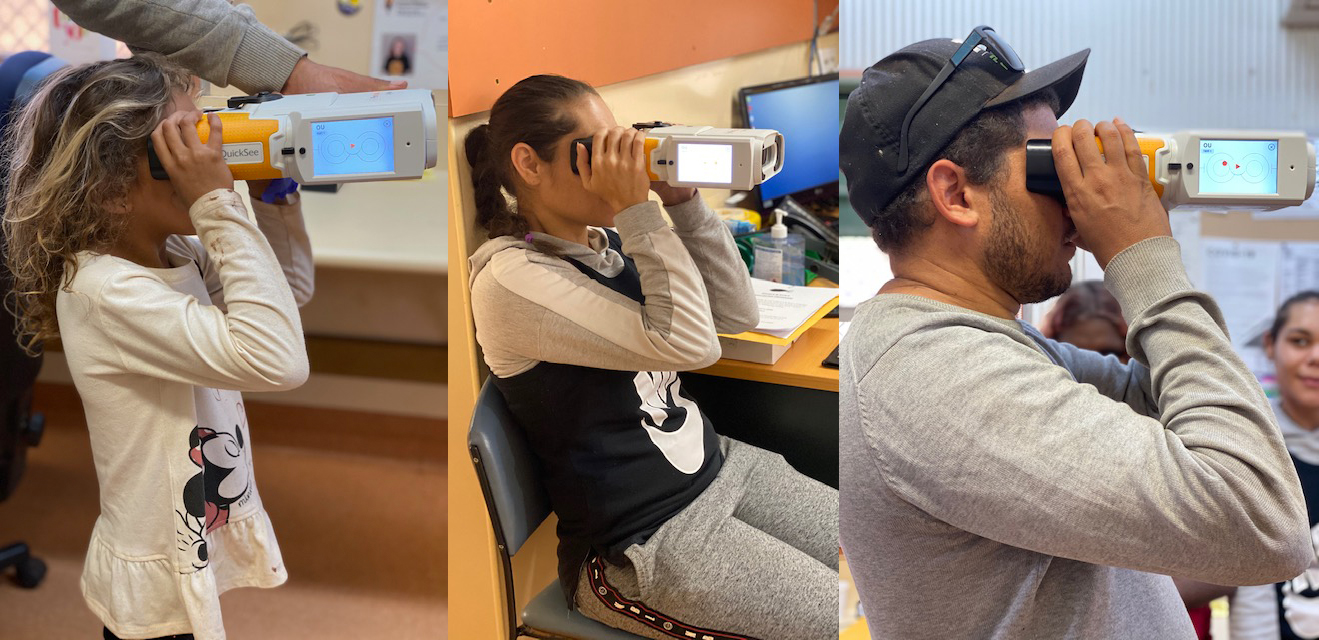
To reach patients, the local nurse practitioner packs all her equipment in a 4×4 and travels to clinics as far as 400 miles (700km). “She carries every piece of equipment we need, so the autorefractor had to be portable and durable,” said Dr Estevez. PlenOptika, he said, “understood the challenges of working in difficult regions, with disadvantaged groups, and what we’re trying to achieve.” That goal: to give people the right glasses via telehealth using QuickSee for a starting point.
This step fit easily into the nurse practitioner’s routine eye exam, and if QuickSee measurements showed the need for correction, she would call or videoconference with Dr Estevez to determine the best treatment for the patient.
According to a study Dr Estevez performed to evaluate the practice outcomes,
“A hybrid teleophthalmology consultation (HTC) model of eye care delivery, which includes both asynchronous and synchronous methodologies…was reliant on three-way interactions using a videoconference platform between patient, healthcare worker and eye care provider. A series of tests occurred prior to optometrist-consultation and include vision assessments (distance and near visual acuities), autorefraction, intraocular pressure, pupil and motility functions and posterior eye imaging. Using a patient-centered framework the results were summarised and discussed with the patient and on-site health care worker, with therapeutic management and referrals made with local coordination support as required.”
They implemented their new practice in June and operated into August. By September, travel restrictions had eased, and Dr Estevez was able to visit the region again. By late fall they had measured about 100 people with QuickSee ranging from school-age children to the elderly. To meet the backlog of patients, he made a few extra visits, but he notes, “we will probably keep going with this hybrid model we created, and that will include the QuickSee. You really need to be solving issues all year round.” It helps, he also said, that Australia’s leading optometry body quickly developed guidelines supporting telehealth practices.
His study concluded, “The implementation of the hybrid teleoptometry model allowed for timely access to eye health services for the population… Although further evaluation and improvements are needed, this model of teleoptometry shows promise for the future in servicing rural Australian communities in adjunct with face-to-face consultations.”
Dr Estevez’s practice innovation helps to fulfill PlenOptika’s founding mission to make excellent vision care available to everyone—especially to those in low-resource settings.
Jose Estevez Bordon, OD
Flinders University
Teleoptometry practice in remote Australia
To preserve the privacy of the community, the region and the nurse practitioner involved in the program are not identified by name.
Please note: Our Privacy policy and Terms of service were updated on September 30, 2025
Are you ready to learn how to use QuickSee Free / Free Pro effectively? Tell us about yourself and your circumstances and we will reach out to arrange a training session with you.